In 1996, Chinese scientists noticed a larger-than-usual number of wild geese dying from avian influenza, a well-known but mild disease that had been found in bird populations for over a century. The outbreak soon spread to chicken farms, where chickens began to die by the thousands. By the time it became apparent that this wasn’t the ordinary avian flu, the first human cases had been reported in Hong Kong.
This new strain of the H5N1 avian flu, dubbed HPAI, for Highly Pathogenic Avian Influenza, appeared to only strike workers on chicken farms. Millions of chickens were culled in order to stop the outbreak, and millions more have been culled during periodic outbreaks in the years since. In 2003, the outbreak began to spread to birds around the world. Today, tens of millions of birds are infected worldwide, including some in the United States and Canada. Commercial turkeys in South Carolina were found to have HPAI just last month.

HPAI kills about half of all humans who get it. Fortunately, it only spreads from bird to person, not from person to person. But when researchers exhumed bodies of survivors of the 1918 flu pandemic (the one that killed around 2% of the world’s population), they found ten mutations the virus had undergone to give it sustained human-to-human transmission. The avian flu, today, has gained eight of those ten mutations. It only needs two more. With its high prevalence in wild birds and abundant opportunities to share genetic material with other influenza viruses, it’s only a matter of time until it becomes transmissible in humans.

This is especially concerning in today’s globalized world. From any starting point, an airplane can reach any destination in the world in less than a day. Ongoing deforestation in the developing world brings ever more humans into close contact with animal populations where pathogenic viruses abound. As the human population has grown billion by billion, so has the population of farmed chickens and other animals we eat. And within many of the world’s largest cities, vast slums accumulate as impoverished people have nowhere else to go, and no way to escape their circumstances. These conditions make our world ripe for epidemics and pandemics, including a pandemic of the avian flu.
Even with draconian quarantine measures, such a pandemic would kill hundreds of millions of people, wiping out a significant fraction of the world’s population in an event dwarfing the death tolls of both world wars combined.
This is real life. Just as the Black Death and the Columbian exchange actually happened, each decimating over half of the populations they affected, the avian influenza pandemic is not a plot from a sci-fi movie, nor is it a half-formed conspiracy theory spreading in dark corners of the internet. This is an event that the world’s leading experts in infectious disease tell us will probably happen, sooner rather than later, unless we drastically scale up our abilities to prevent and respond to global pandemics (more on this below).
It gets worse.

Those two mutations that HPAI needs in order to start spreading in humans? In 2011, Ron Fouchier, a Dutch researcher, gave both mutations to the avian flu virus in his lab. It then easily transmitted between ferrets: a stand-in for humans in the experiment. This caused considerable controversy in the scientific community, especially because no one knew he was doing this until it had already been done. Even the U.S. National Institutes of Health, which had given him the grant for his work, didn’t understand the work’s implications when it gave him the grant. His lab followed standard lab safety procedures to a T, but if it hadn’t—if the virus had somehow escaped, as the plot for so many pandemic thrillers begins—it’s quite possible that half of all people on Earth would have died.
Again, a reminder: this is real life.
Fouchier was disturbingly cavalier about his work. As 80,000 Hours describes:
“Ron Fouchier, when first presenting his work on gain of function avian influenza, did not describe it in terms emblematic of responsible caution, saying that he first ‘mutated the hell out of the H5N1 virus’ to try and make it achieve mammalian transmission. Although it successfully attached to mammalian cells (‘which seemed to be very bad news’) it could not transmit from mammal to mammal. Then ‘someone finally convinced [Fouchier] to do something really, really stupid’ – using serial passage in ferrets of this mutated virus, which did successfully produce an H5N1 strain that could transmit from mammal-to-mammal (‘this is very bad news indeed’).”
It’s true that we need much better international oversight of potentially harmful research and strong public shaming within the scientific community against any researcher who pursues it unilaterally. But even this wouldn’t be enough. When one country forbids such work, a determined researcher can just move to another country. This leads to the Unilateralist’s Curse: even if every scientist on Earth but one believes the research is a bad idea, that one scientist can still pursue it, and potentially cause a global catastrophe.
Fouchier meant us no harm, of course. He was studying the virus as a scientist, and he claims his work is useful for knowing how HPAI might mutate in the wild. The leading journal Science agreed: it published his work for the world to see. The work was replicated in 2013, when Chinese biologists repeated the experiment in guinea pigs instead of ferrets. Once again, arguments about the necessity of the work for learning about influenza were used. (If you’re interested in reading some of these arguments, I recommend this debate between Fouchier and some of his harshest critics that Nature published in 2014.) Most scientists in the field agree, though, that there are ways to gain the same knowledge this research gives us without accepting so much unnecessary risk.
Fouchier’s instructions for how to mutate the avian flu to become human-transmissible are still published online. You can read them yourself here. In fact, the genomes for the Marburg virus, Ebola, smallpox, and many other deadly infectious agents (including, yes, COVID-19) are also available online after a quick Google search.
It gets worse.
In 1987, Japanese biologists noticed mysterious clusters of repeating DNA in E. coli they were working with. The clusters’ function was unknown. Six years later, Dutch researchers found similar repeating clusters in the tuberculosis bacterium. It soon became apparent that these clustered repeats occurred in a whole host of different bacterial species, and they came to be called Clustered, Regularly Interspaced, Short Palindromic Repeats, or CRISPRs. After additional research, we learned that bacteria use CRISPRs to defend against viruses. Each CRISPR is a piece of DNA stolen from a virus that the bacterium once fought and vanquished. When a similar virus tries to invade the bacterium in the future, the bacterium reads from its CRISPRs to find the identical DNA in the virus, then uses a protein called Cas to cut it into pieces and kill the virus.
In 2012, biochemist Jennifer Doudna and her team at the University of California, Berkeley, made the critical CRISPR discovery that changed medical science forever. They programmed a CRISPR (more specifically, the CRISPR’s guide RNA) with DNA that they wanted to cut, and used the Cas9 protein to cut it. This CRISPR-Cas9 system could cut any DNA from any species, including humans.
CRISPR-Cas9 is much cheaper and easier to use than previous methods of gene editing, and has given scientists unprecedented ability to manipulate genetic code. The financial cost of gene editing plummeted in the years after the discovery. We’re still in the early days of CRISPR research, with a vast landscape of possibilities before us. Can CRISPR-Cas9, properly programmed, destroy HIV viruses or cancer cells? Can it stop insect populations from carrying malaria, or even stop them from reproducing altogether? Alarmingly, can it be used to create “designer babies” and change the very definition of what it means to be human? Early research indicates that all of these are possibilities. And improvements to CRISPR systems are being made all the time.
Darker questions quickly present themselves. Can CRISPR systems, and other new tools of synthetic biology, be used to make the avian flu human-transmissible? Can they splice together the genomes of those deadly pathogens so easily found on the internet? Can they be used to build new, wholly artificial viruses from scratch that have never existed in the wild?
The answer to all of these questions is, unfortunately, yes.
CRISPR gene editing is so easy that it’s being taught in many high schools now. And while it takes much more knowledge to actually splice a whole virus genome together and then turn it into a working virus, the tools that’d be used to do this are improving fast. The bar for the education necessary to do it is dropping lower and lower every year. The power to kill hundreds of millions is rapidly slipping away from institutions and falling into the hands of individual people.
If a particularly intelligent college student wanted to combine the high pathogenicity and virulence of SARS and MERS with COVID’s high infectivity and transmissibility, it would be extremely difficult and time-consuming, but it’s not out of the realm of possibility that they could do this, and create a coronavirus that wipes out half a billion people. Fortunately, as of today, most people intelligent enough to do this are mentally stable people.
But certainly not all are. James Holmes, who shot and killed twelve people during a screening of The Dark Knight Rises in 2012, was pursuing a PhD in neuroscience at the time of the mass shooting. He graduated from his undergraduate studies in the top 1% of his class.
Sometime soon, the community of people who want to kill strangers and the community of people who know how to edit virus genomes will overlap, especially as the technology gets cheaper and easier to use. Rob Reid explains this well in his eye-opening TED Talk:
The problem isn’t helped by the multitude of DNA synthesis companies serving the global biology community. Biologists order DNA segments from these companies, and the companies deliver. Unfortunately, the companies will deliver to anyone. In 2006, journalists from the Guardian ordered part of the smallpox genome from one of these companies just to see if they could. The company provided the smallpox DNA as requested, without anyone checking to see who had placed the order.
In the years since, many of the world’s largest DNA synthesis companies, especially in Western countries, have begun to regulate themselves in response to public criticism. But their company policies vary in terms of breadth and depth. In most Indian and Chinese DNA synthesis companies, such self-regulation doesn’t exist at all. International law concerning DNA synthesis also doesn’t exist.
DNA synthesis is much cheaper than it used to be, and the price, currently at about 20¢ per base pair, is dropping constantly. There are 186,102 base pairs in smallpox. If you want to order smallpox’s entire genome in chopped up bits in order to put them back together again, you can do so today, with no legal or regulatory oversight, for $37,220.40.
This is real life.
I admit that I made the title of this blog post up. I don’t know whether we’ll see a pandemic ten times worse than COVID-19 within exactly the next ten years, but given everything I’ve just described, this seems like a pretty conservative estimate. The avian influenza disaster has been brewing for 25 years. We know it’s coming. And the synthetic biology genie is out of the bottle. Within the next couple decades, the power to kill half of humanity will fall in the hands of anyone who wants it.
The problem is clear. So how can we solve it?
There is only one truly permanent solution to the pandemic problem, but it’s probably 30-40 years away, and we need to protect ourselves between now and then, so I’ll describe the permanent solution last. First, I’ll explain some of the ingenious safeguards proposed by the small community of biosecurity experts who have been thinking about this problem, starting with some suggestions for what we as individuals can do. Then, I’ll broaden to a large-scale discussion about what nations and the world can do.
You can prepare for a pandemic the same way you’d prepare for an earthquake or a hurricane: gathering needed supplies and medications in advance. Nez Perce County in Idaho is randomly extremely devoted to pandemic preparedness, and has been since long before COVID. Its emergency management team has put together an excellent, thorough guide for how you and your family can prepare for a pandemic worse than COVID.
Given that mentally unstable people who want to kill others are central to this problem, we can also stop stigmatizing the importance of mental health, especially for young men. Young men are more inclined toward aggressive behavior by a quirk of biology, and society worsens the problem by prohibiting them from showing tenderness or vulnerability, instilling toughness as the ultimate male virtue, and telling many young men that their sole value as a person lies in how much they can earn and how well they can compete.
If we have friends who seem persuaded by the ideologies that most often produce mass murderers today—extreme right-wing, extreme Islamist, and nihilism—we should show them love and try to connect them with mental health professionals. If we need to, we should tell the authorities when we hear someone we’re close to say they’re planning to kill others. It’s tragically shocking how often we hear the words, “I just didn’t think he was serious,” in the aftermath of mass shootings. In general, though, let’s adopt a more compassionate, less punitive approach to these people. We should work together to build a pluralistic society where everyone feels like they’re welcome, like they’re part of a community, and like they can prosper. Psychologists should also prioritize research into malevolence as a personality trait.
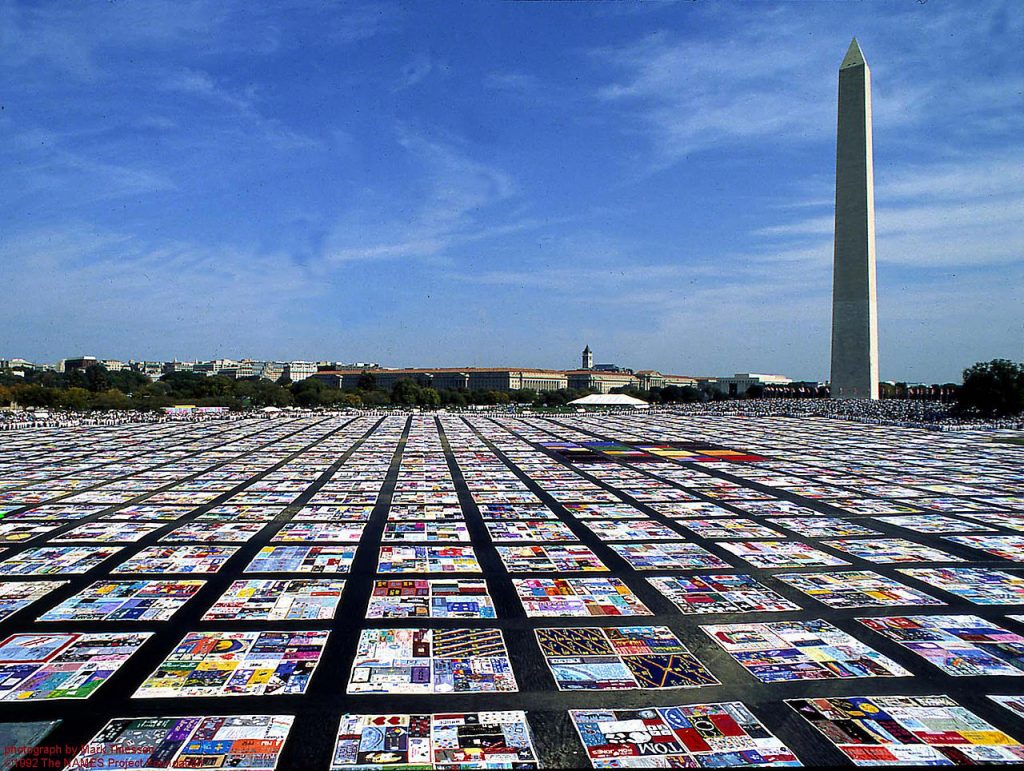
In a similar vein, we should stop thinking that if problems don’t affect us, they aren’t problems. U.S. states with fewer COVID-19 cases had trouble seeing the virus as a threat because it hadn’t affected them as severely as other states yet. Citizens in rich countries have a sad history of apathy toward infectious diseases until those diseases start affecting them, too. The United States barely paid attention to the 2013 Ebola outbreak until it threatened to spill into our borders. When a mysterious virus started killing gay men in the early 1980s, most straight people didn’t care, because it was publicized to not affect them (even though it did, albeit in lesser numbers). Tragically, because HIV is so slow-moving and doesn’t make headlines anymore, it has become a disease we’re content to live with rather than work to eliminate, despite the fact that it’s killed over 30 million people. HIV is truly a pandemic—at this point, the worst in our lifetimes—but because today it mostly affects poor communities and poor countries, many of us don’t care. This apathy toward diseases that don’t affect us must end, and not just because it’s incredibly selfish. It also drastically lowers the speed and the force with which societies are willing to respond to outbreaks, both new and old.
We should also do our best to stop believing misinformation, especially conspiracy theories about how nefarious, secretive groups engineer diseases so they can get more power. During the COVID-19 outbreak, I’ve heard it was the Chinese, it was the U.S. government, it was Bill Gates, it was George Soros, it was Johns Hopkins University, it was doctors themselves, it was a secretive powerful conservative group, it was a secretive powerful liberal group, it was Christians, it was Muslims, it was aliens, it was all of the above working together.
This type of thinking is extremely common during pandemics. Something about this unique type of threat really presses those conspiracy buttons in our brains. During the Black Death, German Christians believed Jews were working at Satan’s behest to spread the disease so they could gain more power; they burned thousands of Jews to death because of this belief. During the European cholera epidemics of the 1900s, commoners believed the wealthy had created the disease to gain more power over the working class. The Zika virus outbreak in 2015 led to accusations in both Brazil and the United States that a “deep state” was using the disease to install a unitary global government. In West Africa during the 2013 Ebola outbreak, many locals thought responders from the World Health Organization were there to harvest their organs.
When humans feel threatened, we seem to have a cognitive bias that’s desperate to pin a face and an ideology on the threat. It’s difficult for our brains to accept that the thing that hurt us was just a force of nature.

Our reaction that there must be an ideology to fight, that there must be a face to hate, must be recognized as an irrational reaction. We need to push it out of our minds. If a pathogen ever were engineered, we’d need all of our reasoning faculties in order to figure out who did it, and we won’t have all those faculties if we jump to the first remotely plausible conclusion that presents itself. It’s possible that in engineered outbreaks in the future, we’ll never know who caused many of them, because it will have been a single individual who died from the very disease they intentionally introduced to the world. In the aftermath, it’s likely that political parties and conspiracy theory groups will prey on our desire to pin a known face onto these threats.
Culturally competent communication from governments during pandemics can go a long way toward assuaging paranoid thinking. A feeling of powerlessness is the psychological kindling for belief in conspiracy theories, so if governments want to foster conditions in which their citizens reject misinformation, they should stop fostering conditions that make so many of their citizens feel so powerless during normal times.
One last thing you can do at the individual level is to go into the field if you’re interested in this problem. The website 80,000 Hours has a great breakdown of the problem and how you can build your education and career toward working on it.
At the global and national levels, there’s a lot of work to do to mitigate future pandemics.
It’s much better to stop these things before they start than to scramble to save lives afterward, but that requires we be proactive rather than reactive. Early detection and containment, case finding (testing), and contact tracing (finding everyone who’s had contact with an infected person) are the mainstays of epidemic response. Right now it takes about twenty days to detect a new outbreak. That time needs to shorten considerably. Early warning technologies like BlueDot and programs like ProMED are extremely useful, but they don’t detect everything, and by the time governments have gotten around to believing their warnings, the disease has already spread.

That’s why it’s so important to shift our global health framework away from disease control programs, and toward building up the health sectors of developing nations. It is absolutely insane that the world depends more on charity organizations than on governments to control epidemics, as if stopping the deaths of millions is something that we, as a species, only get around to if we’re feeling generous. If an avian flu epidemic broke out in Niger today, for example, there’s very little anyone could do about it until it had spread to other, richer countries, at which point it would be far too late to contain the outbreak.
Disease control work from organizations like Doctors Without Borders, the Gates Foundation, and their historical predecessors is immensely laudable and has done untold good. This work, however, is ultimately a Band-Aid for countries mired in poverty and conflict after centuries of exploitation by Western nations. These countries need health systems. Real health systems that can detect diseases as part of their routine course of business, rather than relying on charity workers to fight Ebola or HIV. Charity organizations can only fight outbreaks, and don’t have the resources to change the social, political, and economic conditions that gave rise to Ebola and HIV in the first place. It is the responsibility of the rich nations with histories of exploiting poor nations to help them lift themselves up. Using political and purchasing power to end environmental destruction in developing countries, thus lowering the chances of animal diseases crossing over into humans, would be a great start.
Even in rich nations like the U.S., not everyone has equal access to healthcare, and this too must change. Viruses enjoy economies where, to avoid high healthcare costs, many people only go to the emergency room after they’ve become extremely ill. The U.S. is especially unique in that unlike every other developed nation, it ties each citizen’s healthcare access to their employment status. When COVID-19 hit, millions of U.S. citizens lost their healthcare access along with their jobs right when they needed healthcare most, which made the U.S. uniquely vulnerable to the pandemic among developed nations.
Healthcare access in both poor and rich nations should include mental healthcare. And if the mental health system encounters individuals who talk about killing people, there needs to be an evidence-based, accessible, long-term, rehabilitative care plan for them, rather than legal requirements tying doctors’ hands, throwing mental patients to law enforcement, locking them in a room for a few days or weeks, then turning them back out on their own.

We should also build our healthcare systems to handle extreme events rather than routine events. Many nations run their hospitals at close to full capacity even during normal times, and as we saw with COVID, are totally unprepared for extended surge situations like pandemics. To this end, we need a gargantuan international medical stockpile. Some rich nations, including the U.S., had middling stockpiles of medical supplies that were quickly expended at the beginning of the COVID pandemic. This left later patients, and poorer nations, out in the cold.
More capacity for hospitals and stockpiled PPE supplies sound like important changes to make and maintain when a pandemic is happening right now, and in its immediate aftermath… but funding priorities change during peacetime. We need to find mechanisms to make our leaders stop dismissing long-term risks. Even if pandemics aren’t an immediate concern during a given business quarter or election cycle, money still needs to be spent to safeguard against them. Historically, the U.S. has been pretty bad at this. Biosecurity received windfalls of funding in the wake of the 2001 anthrax attacks, then again after swine flu in 2009, but the funding quickly evaporated once the threat seemed to evaporate.
As is now painfully clear, the threat did not evaporate.

Global organizations should coordinate this preparation for the world, since pandemics are truly global threats. The ineffectual World Health Organization needs to be reformed, and should develop the ability to rapidly send teams of hundreds of response workers to outbreaks. It will need buy-in from all countries in the world to allow this swift response. The world’s nations should also prioritize implementing the Global Health Security Agenda, and strengthen the Biological Weapons Convention. The latter is the organization charged with protecting the world against biological weapons, which has only three full-time employees and funding less than that of a typical McDonald’s restaurant.
Let’s talk medical countermeasures. As is self-apparent to everyone in the world right now, we need the ability to rapidly create and distribute accurate diagnostic tests for new diseases. Preferably, these should be produced so abundantly that they can be shipped within a day of request to people’s houses, and they can test themselves at home. Multitudes of maybe-sick people flocking to hospitals or testing sites, where they’re much more likely to come into contact with the infected, isn’t a great testing strategy in the middle of a pandemic. This capability will largely be determined by test developers. The local governments actually carrying out the testing have little say in the matter.
We also need broad-spectrum antivirals that work well. Broad-spectrum antivirals are medications that can be stockpiled and immediately deployed against novel viruses. We don’t know which virus will cause the next pandemic, and even if we did know, it takes a long time to develop targeted medications. So if we can have a non-targeted medication ready to go by the time the next pandemic hits, we’ll save a lot of lives. Even if it’s only sort of effective, it’ll have that effect on a wide range of viruses, including, hopefully, the one causing the pandemic.
The antivirals we have right now don’t work very well, and they’re very hard to develop. Antibiotics are easy: you just find a drug that kills the bacterial cells and leaves human cells alone. It’s different with viruses, because they’re much smaller than cells, and in fact they live inside cells. Medications that are toxic to viruses are often also toxic to human cells because of this. Fortunately, research in this area is ongoing, and I expect it will get a lot more funding after the COVID pandemic passes.
A universal influenza vaccine would be nice, too. This would be a vaccine that’s effective against all possible incarnations of the flu—past, present, and future—and would at least protect us from avian influenza, our most likely near-term adversary (after COVID). This vaccine has been in development for years, with only mild progress. The United States actually has an unknown quantity of avian influenza vaccine stockpiled, but this vaccine was based on a past version of the virus, and may not be effective at all against a future outbreak strain.
In general, though, we need to move our medical countermeasure development away from countermeasures for specific diseases and toward general countermeasures that would work against any disease. The possibility of designer pathogens in the future makes focusing on “Disease X” urgent. Much of our current efforts focus on countermeasures against the agents on the NIAID’s Priority Pathogens list, especially anthrax, but the next pandemic may not be caused by a known pathogen, even if it comes from a natural source, as we’ve seen with COVID-19.
As Bill Gates advocated in his Ted Talk, we need Germ Games. Like war games, but germ games. Stakeholders at every level of organization—global, regional, national, province-level, county-level, and local—should hold regular exercises to prepare their personnel and decision-makers for pandemics of all severity levels. Clade X and Event 201 were great starts at the national level, and I hope these kinds of exercises spread to all nations, and all levels of organization.
And then there’s the private sector. What’s their role in all this? It’s very important that governments give businesses some leeway and don’t try banning CRISPR and other synthetic biology technology overall, because CRISPR has enormous potential to do good and save lives (it may have already cured glaucoma, for instance), in addition to the tremendous harm it could cause. In fact, CRISPR-Cas systems can be used to fight the very nightmare viruses they can be used to create. Governments shouldn’t overdo regulations on the private sector. Doing so would precipitate hostile relationships with the companies and scientists we’re most trying to get on safety’s side. Mutually beneficial partnerships with businesses are a must.

We need international laws and enforcement mechanisms to be put in place for DNA synthesis companies, and we should develop cheap technology to screen their DNA orders. We also need better security in biolabs. Pathogens, occasionally including very serious, highly lethal pathogens, go missing or get loose from biolabs all the time. You’ll find a plethora of stories if you Google this, but I’ll highlight here that even the labs at the CDC, some of the safest in the world, have had accidents with anthrax and smallpox.
Shockingly, no biolabs in the United States are required to carry insurance against such accidents, and so receive no financial feedback about the risks they may be taking. We need mandatory insurance for labs, mandatory notification laws concerning safety breaches, and incentives to financially reward whistleblowers. We need to find ways of implementing these changes that biolabs themselves will agree to, and that won’t overly burden them. And these changes should apply to all biolabs in the world via international treaty.
Every government and business should have a pandemic plan. Lives depend on the economy, so we need plans to sustain economies and markets during quarantine. All organizations should know how their operations will continue, and have continuity plans if people in key positions get sick or die—especially a consideration for medical services. We need to diversify and decentralize supply chains, especially for stuff like medical supplies, much of which came from China before the outbreak.
Those famed three months of personal emergency funds that everyone is supposed to save up, just in case? All employees of large companies should be paid well enough, indexed to the local cost of living, that they can afford to save up those funds in the first place. U.S. megacorporations are much richer than most people think. They can afford it to the point that I’m comfortable with this being an exception to my “don’t overburden the private sector” rule.

Unfortunately, we need to plan for pandemics much worse than COVID-19. Pandemics so bad that we’ll need to worry about a large fraction of the response workforce, including vaccinologists, virologists, doctors, and nurses, succumbing to the disease, thus removing their knowledge and experience from our society when we need it most. Pandemics so bad that grocery stores have to close, and we need to figure how else people will get food. Local governments need to stockpile not only medical supplies, but also non-perishable food. Pretty dark, huh?
There’s a light at the end of the tunnel. With enough investment and effort, this is a solvable problem. To solve the big pandemic problem, we need to solve a smaller, but still giant, more technical problem: how to develop and mass-produce vaccines very, very fast, without eggs.
It takes a long time to make a vaccine. It’s been forty years since we discovered HIV, and we still don’t have an HIV vaccine. In the 2009 swine flu pandemic, creating a vaccine took six months, but that’s only because the entire vaccine industry was built around the influenza vaccine in the first place. Influenza is the one vaccine we all need every year, so the market has prioritized its production above all other vaccines, including Disease X. As soon as something that’s not influenza comes along—say, maybe, a coronavirus—the vaccine industry gets knocked on its butt and has to build new infrastructure, workflows, and science from scratch.
The vaccine creation process clearly needs to be generalized for Disease X, but it also needs to become faster. To make a vaccine today, the pathogen is inserted into fertilized chicken eggs, which it infects. Once it’s reproduced itself enough inside of the egg white, the egg white is extracted, and the virus within it chemically inactivated. This inactivated virus is the vaccine.
This is only one of many ways of making vaccines, but they all involve chicken eggs, which is the important part. The supply of vaccines is limited by the supply of eggs. If the entire world’s population needs a new vaccine all at once, you sure as hell had better have four billion chicken eggs ready to go. (One egg produces two doses of vaccine.) And they have to be perfectly sized eggs, too, since they’re handled by robots that would drop or crush eggs of slightly different sizes. And then the vaccine needs to go through clinical trials to prove it’s safe and effective.
These logistical problems aren’t insurmountable, but they carry a fatal flaw: they make the process very, very slow.
Enter the Gates.

You know, the couple that singlehandedly caused COVID-19 so they can cull the human population and take over the world. Those Gates.
The Gates, along with some top vaccine researchers, recognized that solving the vaccine problem would also solve the larger pandemic problem. If you could create and mass-produce a vaccine for a totally new, unknown disease within days of an outbreak and distribute it globally, no pandemic would ever threaten the world again. The Gates also recognized that no government or business was doing any work to solve this critical problem. No nonprofit organizations were working in this space.
So they created one.
The Coalition for Epidemic Preparedness Innovations, or CEPI, began operations in 2017, funded by Japan, Norway, Germany, India, and the Gates Foundation. The pharmaceutical industry’s failure to quickly create an Ebola vaccine during the 2013 Ebola outbreak, largely driven by the fact that it had no financial incentive to do so, prompted these altruistic governments to participate. CEPI’s primary goal is to develop vaccines for a handful of the diseases that experts believe are most likely to cause future pandemics. Thrillingly, two of the diseases it’s been working on are SARS and MERS, two cousins of COVID-19, and CEPI is now working swiftly to apply its research into those vaccines to a new COIVD-19 vaccine. But CEPI also has the longer-term goal of radically reducing the time it takes to create, mass-produce, and distribute vaccines. It takes ten years on average to do this for vaccines today, but CEPI aims to be able to create a million vaccine doses for a new disease within thirty weeks of its first case.
Even this may not be fast enough to stop a pandemic before it starts, but it’s a bold step in the right direction. It will probably take at least three decades of well-funded research to get vaccine development fast enough that the world will be forever protected from pandemics. But that is the ultimate solution. And more funding would help. We need a “moonshot” for making vaccine development faster. Our lives may depend on it.
At CEPI’s launch, its leaders promised equitable access to any vaccines it produced: people in poor countries would have access to them without being charged a lot of money. There is some concern that CEPI’s alliances with major pharmaceutical companies have undermined this initial commitment, which is unfortunate. To prevent a pandemic, a vaccine distribution system must be truly global, and it can’t rely on global market forces, which primarily serve rich countries for the time being. Both practically and ethically, vaccines produced in response to a pandemic should be easily accessible to everyone in the world, both poor and rich.
How do we get vaccines to people faster? The production process can be sped up by using bacteria instead of chicken eggs to mass-produce vaccines, although there’s been very little research in this area and we have a lot of progress to make. If we can make perfect computer models of viruses and human cells, we may even be able to design vaccines in a computer and 3-D print them into existence. This seems like impossibly advanced science fiction now, but with artificial intelligence poised to revolutionize healthcare just as much as CRISPR, it may be possible in the coming decades.
Vaccine factories should be generalized to produce any type of vaccine that might be needed, not just influenza vaccines. And they should be built all over the world, by a variety of companies, to establish regional vaccine supply chains and end the world’s vaccine dependence on a handful of Western nations. Alternately, widespread biological printers could be installed at hospitals everywhere, so vaccine blueprints could be digitally sent and hospitals could become their own suppliers. (The use of these machines would need to be heavily guarded to prevent abuse by nefarious actors.)
If we could get vaccines to the world so quickly, would this truly be a permanent solution to pandemics? Couldn’t a terrorist still create a completely novel virus that scientists have no frame of reference for when developing a vaccine, stretching the development timeline out once again? It’s possible. And this is why it’s urgent that we catalog as many natural viruses as we can, to learn about a broader range of what types of viruses can exist. Most viruses on planet Earth remain undiscovered. We also need to invest in educating a large, permanent workforce of virologists and vaccinologists to staff this new global vaccine system and decode any mystery viruses that bad people throw at us.
There will always be more of us than there will be of those bad people. As the world grows more ethical and the circle of empathy expands, we’ll outnumber them even more. As long as our commitment to guarding against pandemics continues, I think we’ll be able to stop them as soon as they start.
We’ll be able to, that is, if we can make it through the next 30-40 years, until fast vaccine technology gets developed.
Let’s get preparing. The clock is ticking.
If you’re interested in learning more about pandemic mitigation, I can’t recommend the 80,000 Hours website enough. I learned a good third of the information in this post from them.
Note: For the sake of brevity, I simplified some of the information in this post so that it’s not precisely accurate. I made only minor changes to accuracy, however, and none would alter or distort the arguments I make above. If you feel anything in this article is misleading, please contact me and I will make my best effort to correct it for accuracy in accordance with expert consensus.